Malaria is a serious and sometimes fatal tropical disease. Four kinds of malaria parasites can infect humans: Plasmodium falciparum, P. vivax, P. ovale, and P. malariae; infection with P. falciparum, if not promptly and correctly treated, can be fatal in as little as one or two days.
Competent advice from an up-to-date source of information, such as the tropical diseases department of a major hospital, is essential.
Understand
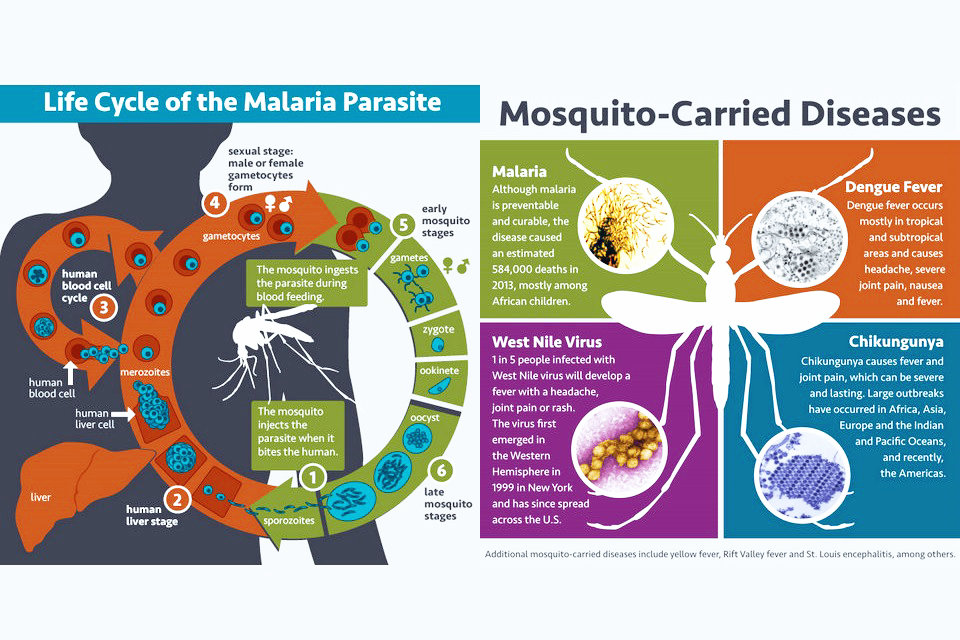
The parasite responsible is a protozoan dixene (that is to say, requiring an intermediate host, in this case the man, and a definitive host, in this case the mosquito, during its life cycle) called Plasmodium and of which only 5 of the 150 existing species are involved in human pathology. Four species are responsible for a benign form of the disease and one species ( Plasmodium falciparum ) of the malignant form that can lead, without treatment, to death. Be careful however that the benign forms should not be taken lightly because sometimes it can lead to death especially if the patient also suffers from another pathology.
The human form of this parasitosis is almost as old as humanity and has been affecting it for more than 50,000 years . Analyzes performed on his mummy have, moreover, proved that Pharaoh Tutankhamun was suffering from malaria at the time of his death.
Some classify malaria as tropical diseases, which is not entirely accurate. The confusion stems from the fact that it has been eradicated from Europe and North America. She was so well known in England in the xvii th century, William Shakespeare speaks in eight of its parts. It raged until 1958 in the polders of Belgium and the Netherlands and the last epidemic experienced by Corsica took place between 1970 and 1973.
Transmission
Malaria is transmitted when an infected mosquito bites a human. The mosquitoes that can carry Plasmodium parasites are mostly active during dusk and dawn as well as at night. The best way to avoid infection is not getting bitten in the first place.
As stated by the CDC, malaria is transmitted in large areas of Central and South America, the island of Hispaniola (which includes Haiti and the Dominican Republic), Africa, Asia (including the Indian subcontinent, Southeast Asia and the Middle East), and a few areas of the South Pacific.
In general, the risk of contracting malaria is higher in rural areas and lower in urban areas. Often there is also a correlation to the mosquito population, with the rainy season creating stagnant pools of water where mosquitoes can breed. Many cities in tropical areas were founded at elevations where mosquitoes are or rather were rare; however, with climate change, this is beginning to change in some places.
Diagnosis
The only really effective way to determine the presence of Plasmodium and to know what species it belongs to is a blood test under a microscope.
Symptoms
Symptoms of malaria mimic common flu, with an infected person suffering fever, headache, and vomiting usually within 10 to 15 days after the mosquito bite. This means that you may become sick when you’re already back at home.
Malaria is life-threatening, and requires immediate treatment. No vaccine is commercially available as of 2018, but methods of prevention include avoiding mosquito bites and preventative drugs (prophylaxis). Some drugs are not effective for all areas. If a person who has visited a malaria risk zone contracts a fever within one year, their physician should be informed of the possibility of malaria. Less serious forms (such as P. vivax) can mimic symptoms of the flu. Physicians who rarely, if ever, examine malaria patients may need to be reminded of this fact. The standard laboratory test for malaria is a thick and thin blood smear on a glass slide viewed under the microscope. Self-test kits are highly unreliable.
This periodicity of febrile recrudescences is the best way to make a first sort to know what Plasmodium you have to do, as far as malaria is concerned and only this one.
“Quarter fever” because having a periodicity of feverish states every three days:
Plasmodium malariae which causes a mild form but which can be durable or even chronic;
“Third fever” because having a periodicity of feverish states every two days:
Plasmodium falciparum , it is he who causes the malignant form,
Plasmodium oval that causes a mild form. Rarer than the others, it is only found in certain areas of tropical Africa,
Plasmodium vivax which causes a benign form;
“Continuous fever” because having a periodicity of feverish states every day:
Plasmodium knowlesi that causes a mild form. However, it is only found in Asia and more particularly in Southeast Asia.
Although P. knowlesi only occurs in Asia, continuous fevers can be observed in all regions of the world. This may mean that the female mosquito has simultaneously inoculated two different Plasmodium species or a malaria parasite and a virus or that the patient has both malaria and typhoid or paratyphoid fever.
A hemoptysis is not a symptom of malaria. This is due to the repetitive coughing effort that occurs mainly in asthmatics or children who produce a psychosomatic reaction to their general poor health.
Clinical signs
The main clinical signs are: fever over 40 ° C , intermittent tremor, joint pain, signs of anemia caused by the destruction of red blood cells, the presence of hemoglobin in the urine, a decrease in arterial blood supply to the brain (explaining headache), impaired renal function, seizures and jaundice. Other less common signs are increased volume of the spleen and / or liver (in the case of the liver, the increase is easily palpable under the right rib margin) as well as hypoglycemia.
Prophylaxis
The best prophylaxis against malaria is to prevent being bitten by mosquitoes, particularly at night when the Anopheles mosquitoes are active. Not in every malaria area does accommodation offer mosquito nets, so best bring your own net. If the next proper hospital is not further away than a day’s journey, taking preventive medicine might not be worth the risk of side effects. However, malaria can incapacitate a person within hours, so if only one person can drive a car, prophylaxis should be considered for them.
Any malaria prophylaxis must be taken before, during, and (especially) after travelling to a malaria-risk zone. Anti-malarial drugs are highly effective in preventing malaria. Different drugs are recommended for travel to different areas due to malarial strains resistant to certain drugs. Talk to a specialist doctor or verify the information with a reliable source. As with all drugs, anti-malarials may cause side-effects. Seldom will malaria be the sole health concern, and the physician will need to assess all the health risks the traveller will face. Obtain medications from a reliable source, either at home before you leave or from a reliable chemist/pharmacist in a high-end or tourist area. Sometimes, the pills sold might be placebos.
Medical prophylaxis that contains mefloquine can have serious psychological and neurological side effects (anxiety, headaches, insomnia, dizziness) that incapacitates about 11-17% of travelers to some degree. Pregnant women should be especially careful, as some anti-malarials must not be taken during pregnancy. Malaria during pregnancy is usually more severe, and it’s always considered to be a serious emergency. As with most prophylaxis, anti-malarials are not 100% effective; however, studies have shown that, when taken as directed, the most common drugs (e.g. doxycycline, Malarone) are about 98-99% effective. The choice of a malaria prophylaxis should be made carefully with one’s physician, taking into account drug resistance in the traveller’s destination; possible side effects, interactions, and contra-indications; and finally the preferred frequency per dose (daily, weekly, etc.)
As well as prophylactic medications, there are important anti-mosquito measures that should be used. Avoiding mosquito bites by using repellent containing DEET, netting, screens, long clothing, and avoid being exposed around dusk. Permethrin-treated fabrics kill mosquitoes. Air-conditioning and fans can also help indoors. For those sensitive to DEET, or who dislike its smell, repellents containing Picaridin (e.g. Natrapel) are available in limited areas. Concentrations of 20% have been shown to be as effective as DEET.
The most common anti-malarials include:
Doxycycline is highly effective and can be very inexpensive. Possible disadvantages include increased sun sensitivity (sunburning easier), and nausea and stomach pain; some sources caution that it may reduce the effectiveness of birth control pills.
Lariam (mefloquine) or its generic, Mefliam, is highly effective, has a simple weekly dose and can be taken for extended periods. It does have a number of contra-indications and must be prescribed by a doctor, and has also been known to have very rare but severe neurological side effects. More common side effects include nausea, stomach cramps and lucid dreams. Not to be used if you plan on scuba diving or high-altitude climbing. Your doctor may advise starting using it several weeks before departure, in order to check for possible side effects. There are resistant mosquitoes in Southeast Asia, and West and East Africa. Find out the latest information on this drug from a professional before purchase.
Malarone (atovaquone + proguanil) is highly effective, has a very low incidence of side effects, and only needs to be taken for one week after leaving the risk area; however it is the most expensive.
Chloroquine (Daramal, Nivaquine, or Promal) in combination with proguanil (Paludrine) may sometimes be recommended, and is generally well tolerated. Problems include people having difficulty adhering to the prescribed regime due to its complexity, and widespread resistance.
There has been some debate over whether pre-travel malaria prophylaxis is being started early enough. For example, mefloquine is normally taken one week prior to travel. Some feel this is inadequate if the person is unfortunate enough to be exposed to malaria shortly upon arrival. Those who have concerns may wish to discuss with their physician the option of doubling the time period (not the dosage) that their malaria prophylaxis will be taken prior to travel. In addition to providing better protection, there will be more time to switch to another anti-malaria medication, if necessary.
Aspirin must never be taken as an antipyretic (fever reducer) when malaria or dengue fever is a possibility. (Continuing daily low-dose 81mg aspirin therapy during and after third-world travel should be discussed with your physician.) Acetaminophen (paracetamol) and ibuprofen are considered safe alternatives provided all of their precautions are observed. Malaria, dengue fever, and typhoid fever all tend to have somewhat similar symptoms at first, and should not be self-diagnosed.
Therapy
The only currently valid treatment is a combination artemisinin-based combination therapy ( ACT ). This drug combines a derivative of artemisinin, which acts very quickly against the parasite but also quickly disappears from the body, and another molecule deemed antimalaric, which slower to react, is supposed to eliminate what the derivative of artemisinin would not have done. It occurs either in tablet form or as an intravenous injection (for cases where the patient is unable to ingest) and the treatment lasts for three days.
There are dozens of drugs on the market that combine different combinations. They are generic and available worldwide. It is the doctor, and he alone, who decides on the most appropriate combination to use.
The main contraindication to this therapy is the treatment of pregnant women and infants under nine months of age.
ACT – List of ACTs approved by WHO.
If an ACT is not available directly, taking the prophylactic drug in your possession is entirely adequate but the new doses should be determined by a doctor and discontinued as soon as an ACT is available.
Travel
Travel to rural areas always involves more potential exposure to malaria than in the larger cities. (This is in contrast to dengue fever where cities present the greater risk.) For example, the capital cities of the Philippines, Thailand and Sri Lanka are essentially malaria-free. However, malaria is present in many other places (especially rural areas) of these countries. By contrast, in West Africa, Ghana and Nigeria have malaria throughout the entire country. However, the risk is much lower in the larger cities. Always use up-to-date information as to whether malaria is present in the areas you will be visiting, and what prophylactic resistance occurs locally. A small map of the world (above) cannot show small pockets of malaria-free zones (which are likely to be prime tourist areas and/or larger cities). Conversely, sometimes malaria spreads into new territory—especially higher elevations near endemic zones.
Travellers should never assume that their choice of malaria prophylaxis is available in the country that they will be visiting. Many third-world countries stock only chloroquine and possibly doxycycline and there is also a risk of buying fake drugs. Quinine (a natural drug, and known for centuries) might also be available, but is not recommended as a prophylactic anti-malarial. Resistance to it is extremely common.
Protection against the vector
Avoiding malaria means first avoiding mosquito bites by taking a few precautions.
sleeping under a mosquito net with a mesh size of less than 1.5 mm and, if possible, impregnated with insecticide, which will protect the body parts that come into contact with the mosquito net. It is also imperative to check, every evening before bedtime, if the mosquito net is in perfect condition;
use an insecticide inside not forgetting the underside of the bedding and furniture. Thus Anopheles gambiae , which is one of the main propagators of malaria, is attracted to Kairomones (volatile or mobile semiochemicals produced by a living) from the feet and ankles and used to fly low to the ground;
mosquitoes being sensitive to the movement of air, the action of a fan, even if the room is equipped with an air conditioning system, will also be part of the means of protection;
at sunset, coat the permethrin garments or the skin with a repellent consisting of a solution containing 30% DEET for adults or 10% of the same product for children between 2 and 12 years of age;
after sunset, wear loose, long, light colored clothing and, if possible, refrain from drinking alcohol. Anopheles are also attracted by dark colors, especially black, than by alcohol vapors.
Beware that if females of anopheles, malaria spreaders, are active between dusk and dawn, females of other mosquito species, propagators of viruses such as Zika fever , chikungunya , dengue fever or yellow fever are active during the day. The same precautions are therefore desirable in the daytime.
Protection against the parasite
Since July 2015, there is a vaccine for children aged between six weeks and seventeen months, the Mosquirix TM developed by GSK . However, this vaccine, also anti- hepatitis B , is currently available only in areas where malaria is endemic.
The only global protection against parasites is the taking, at the time of a meal, of a prophylactic drug adequate to the zone of chemo-resistance of the parasite:
zone 3 countries:
Malarone® one tablet daily, one day before departure and up to seven days after return . box of 12 tablets – Belgium: 30,9 € for adult and 18,48 € for junior – France: free price with an average of 35,38 € for adult . – Information about the medicine .
Lariam® one tablet a week, two to three weeks before departure and up to four weeks after return . box of 8 tablets – Belgium: 34,26 € – France: free price with an average of 38,47 € . – Information about the medicine .
zone 2 country:
a combination of chloroquine and proguanil
Nivaquine® one tablet daily, one week before departure and up to one month after return . box of 100 tablets – Belgium: 4,66 € – France: 9,14 € . – Information about the medicine .
Paludrine® two tablets daily, one week before departure and up to one month after return . box of 56 tablets . – Information about the medicine .
Zone 1 country :
Nivaquine® Logo indicating schedules one tablet daily, one week before departure and up to one month after return . Logo indicating rates box of 100 tablets – Belgium: 4,66 € – France: 9,14 € .
These medications must be prescribed by a doctor who will also determine the doses to be taken according to the weight of the traveler and according to a state of pregnancy in progress. He can also advise you other recommended medications and vaccinations recommended according to the news of the country you are visiting. If you want to have the time to vaccinate, the medical check-up must be done two months before the trip.
Remarks
If you have headache, intermittent fever ( 38 ° C or higher), vomiting, diarrhea, or bloody urine , within 8 days to several weeks after returning from an at-risk area , see doctor. The care by a doctor must be fast.
As preventive treatment is not covered by Social Security, plan a budget accordingly.
A trip to an area at risk of malaria temporarily excludes you from donating blood.
Be careful that if you have received a live strain vaccine (especially against typhoid ), taking an antimalarial prophylactic drug can start at least three days after vaccination.
Beware that if a co-infection with the human immunodeficiency virus (HIV) does not increase the risk of mortality, they each contribute to their mutual spread: malaria increases the viral load of HIV and HIV infection increases the probability of a malaria infection.
Find out more
WHO – Malaria. World wide information on malaria from the World Health Organisation.
MAP (Malaria Atlas Project)
MARA (Mapping Malaria Risk in Africa), a malaria atlas for Africa. Requires registration.
South African Department of Health
The National Health Service in Scotland publishes maps showing malarial hotspots
IAMAT (International Association for Medical Assistance to Travellers) Malaria information, white paper, and risk chart for travellers